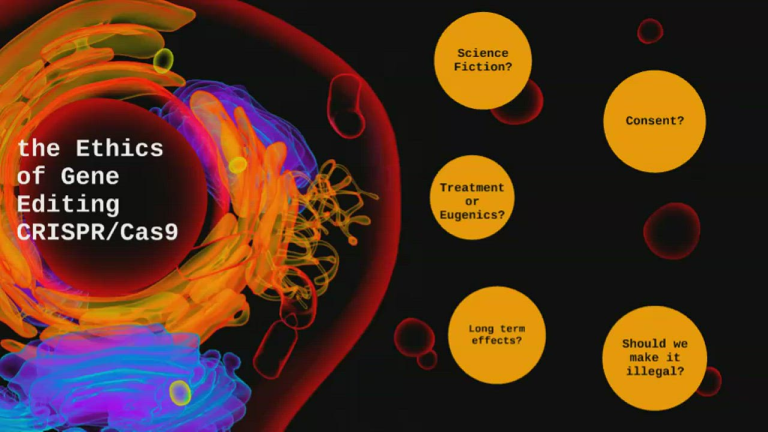
The ethical implications of CRISPR are at the forefront of conversations surrounding gene editing technologies today. As scientists explore the potential of CRISPR technology to cure diseases such as sickle cell disease, many grapple with the moral questions it raises about human intervention in genetics. Should we embrace such powerful gene editing tools with open arms, or do we risk crossing ethical boundaries that could redefine our understanding of health justice? These discussions echo the broader concerns of medical ethics, urging us to reflect on the responsibilities that come with the ability to manipulate the very fabric of life. With the promise of curing debilitating conditions comes the potential for unforeseen consequences, pushing society to critically address the implications of our choices in biotechnology.
In recent years, discussions about the transformative power of gene manipulation technologies, notably the CRISPR-Cas9 system, have gained significant traction. This revolutionary method of altering genetic material has opened a Pandora’s box of possibilities, particularly in treating hereditary conditions like sickle cell anemia. However, the inquiry extends beyond mere medical outcomes, encompassing a range of ethical dilemmas associated with genetic customization and enhancement. The potential for these tools to influence notions of health equity adds weight to the debate surrounding bioscientific innovation. As we navigate this complex landscape, it’s crucial to scrutinize who benefits from such advancements and the broader societal impacts of our choices regarding genetic health interventions.
Understanding CRISPR Technology
CRISPR technology is a groundbreaking innovation in gene editing that allows scientists to alter specific genes within living organisms. It stands for Clustered Regularly Interspaced Short Palindromic Repeats and works alongside a CRISPR-associated protein, particularly Cas9, to create precise changes in DNA sequences. This technology has made significant strides in treating genetic disorders, with sickle cell disease being a notable example. The ability to edit germline cells means that genetic modifications can not only prevent the disease in future generations but also provide immediate relief to patients, prompting discussions about the transformative potential of CRISPR at a genetic level.
The implications of CRISPR are vast, not only in the realm of medicine but also in the ethical considerations that accompany such powerful tools. As we explore the applications of CRISPR technology, it is essential to examine whose interests are being served. With a diverse range of potential applications, from curing hereditary diseases to potentially enhancing human traits, we must ask ourselves: how do we navigate the moral landscape of gene editing? This question stands at the forefront of medical ethics today, particularly as we consider the rights of parents versus the autonomy of future individuals.
Ethical Implications of Gene Editing
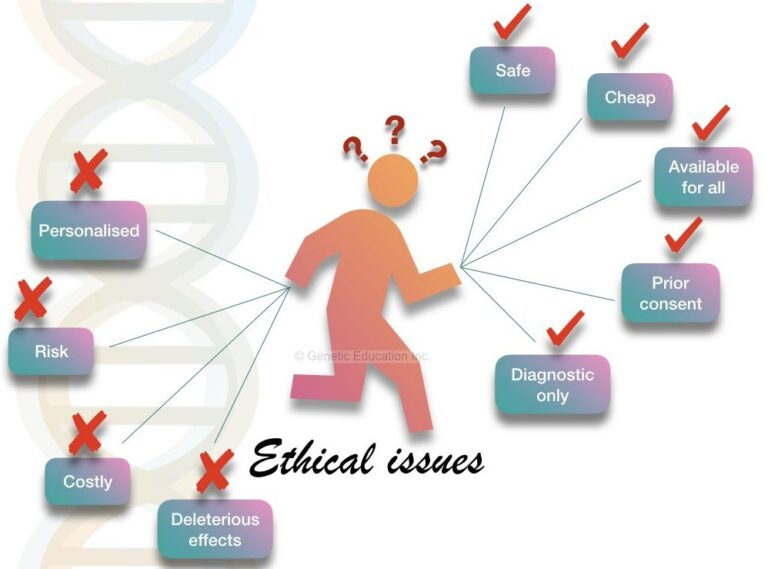
The ethical implications surrounding gene editing with CRISPR are profound and multifaceted. At the heart of this debate lies the question of human enhancement versus disease prevention. For instance, while the ability to cure sickle cell disease brings hope to many, it also raises concerns about the potential for gene editing to be misused for non-therapeutic enhancements. Should parents have the right to decide the traits of their children? As society advances in its capabilities to edit genes, the lines between health, enhancement, and what it means to be human blur, creating a controversial debate within medical ethics.
Furthermore, the conversation about CRISPR inevitably touches upon health justice. The accessibility of gene editing technologies is critical; the exorbitant costs associated with CRISPR treatments may widen the health disparities gap. For diseases like sickle cell anemia, which predominantly affects underserved populations, ethical questions regarding who receives treatment and who is left behind become paramount. If only a wealthy few can afford gene editing, the promise of equality in healthcare reform risks being undermined. This highlights the urgent need for a framework that integrates ethical considerations into the development and distribution of gene editing technologies.
Health Justice and CRISPR
Health justice is an essential aspect to consider within the context of CRISPR technology. The advancements in gene editing bring immense hope for curing genetic diseases, but they also challenge existing systems of healthcare equity. As highlighted by experts in the field, it is crucial that innovations in gene editing do not benefit just those with the means to pay. The cost of CRISPR treatments, such as the approximately $2.2 million cure for sickle cell disease, raises significant questions about fairness and access across different socio-economic groups.
To truly embody health justice, stakeholders must ensure that advancements in medical technology like CRISPR are translated into broader societal benefits. This involves not only making treatments accessible and affordable but also addressing systemic inequalities that prevent marginalized communities from reaping the benefits of scientific progress. As the conversation about CRISPR continues, it is vital to include diverse perspectives and advocate for inclusive policies that prioritize equitable healthcare access for all, especially those most impacted by genetic diseases.
The Role of Medical Ethics in CRISPR
Medical ethics plays a critical role in guiding the responsible use of CRISPR technology in healthcare. The potential to edit genes raises fundamental ethical dilemmas that medical professionals, scientists, and policymakers must navigate carefully. As discussed in various academic forums, the distinction between therapeutic interventions and enhancements becomes increasingly nebulous, presenting challenges in how ethical standards are applied. Decisions on whether to use CRISPR for conditions that do not significantly impair the quality of life, such as certain genetic predispositions, must be approached with caution and deliberation.
Moreover, the need for rigorous oversight cannot be overstated. Current regulations surrounding gene editing differ significantly across countries, and the lack of a global consensus raises concerns about unethical practices. For instance, while it is prohibited to perform germline editing in several nations, this may not be the case in others. This disparity calls for an international framework that enforces ethical guidelines and monitoring to ensure that CRISPR is used responsibly and equitably. As we continue to innovate in gene editing, an unwavering commitment to ethical standards will be paramount in shaping a future that respects human dignity and diversity.
Potential Risks and Unintended Consequences
While CRISPR technology holds immense promise for treating genetic disorders, it also presents potential risks and unintended consequences that warrant careful consideration. For example, gene editing is a highly complex process that may lead to off-target effects, where unintended genes are modified. This could potentially result in unforeseen health issues, raising questions about the long-term safety of such interventions. As scientists push the boundaries of gene editing capabilities, ensuring a thorough understanding of these risks is essential to safeguard patients.
Additionally, the implications of CRISPR extend beyond immediate health concerns. The manipulation of genes could alter ecological balances or create unexpected biological interactions, prompting worries about ecological ethics. The effects of altering a single gene can ripple throughout an entire genetic system, posing challenges to our understanding of complex biological interactions. As research progresses, it is critical that researchers prioritize transparency, engage in robust peer review, and involve diverse stakeholders to mitigate risks and foster responsible innovation in the field of gene editing.
The Future of Gene Editing and Policy
The ongoing advancement of CRISPR technology presents opportunities for transformative changes in healthcare policy. As gene editing becomes more prevalent in treating diseases like sickle cell, it raises the imperative for lawmakers and healthcare professionals to devise policies that balance innovation with ethical standards. The discussion surrounding the governance of gene editing is becoming increasingly vital, as stakeholders seek to ensure that developments in biotechnology align with societal values and ethical principles.
Effective policy frameworks will need to address not only the regulation of scientific practices but also the equitable distribution of gene therapies. This includes ensuring that marginalized communities have access to cutting-edge treatments without financial burdens. Policymakers must also consider the social implications of gene editing, evaluating societal perceptions of genetic modifications and the need for extensive public dialogue. By proactively establishing guidelines that incorporate ethical, health justice, and safety considerations, society can navigate the complexities of gene editing while harnessing its full potential.
Diverse Perspectives in CRISPR Discussions
In the realm of CRISPR technology, diverse perspectives are essential for a well-rounded understanding of its implications. Engaging voices from various fields—including bioethics, genetics, sociology, and law—can enrich the discourse surrounding gene editing. These multifaceted discussions are crucial for addressing the moral and cultural dimensions of modifying human genomes, particularly when considering the potential for disparate impacts among different communities.
Furthermore, incorporating the lived experiences of individuals affected by genetic conditions can deepen our understanding of the ethical landscape. For instance, those living with conditions like sickle cell disease or other genetic disorders can provide insights on the implications of gene editing on identity, quality of life, and individual autonomy. Involving patients, advocacy groups, ethicists, and policymakers in collaborative dialogues will foster more inclusive and empathetic frameworks for discussing the responsible use of CRISPR technology.
The Intersection of Technology and Humanity
The conversation surrounding CRISPR underscores the profound intersection of technology and humanity. As we push the boundaries of what is scientifically possible, we must remain acutely aware of our humanity and the ethical standards that uphold it. The potential to eliminate genetic diseases raises critical questions: at what point do we intersect the line that separates progress from playing God? The very essence of what it means to be human is rooted in our genetic diversity, and as we explore the capabilities of CRISPR, we must reflect on the implications for personal identity and societal norms.
This intersection also highlights the importance of individual agency in genetic modifications. Technology gives rise to possibilities that were previously unfathomable, yet it concurrently demands rigorous ethical scrutiny. Balancing innovation with compassion and responsibility is paramount as we navigate the uncharted waters of gene editing. The fundamental principle of ‘do no harm’ will serve as a guiding light for scientists and society alike in determining the most ethical approaches to utilizing CRISPR technology in the future.
Navigating Global Perspectives on Gene Editing
As CRISPR technology evolves, it becomes increasingly critical to navigate global perspectives on gene editing. International differences in regulations and cultural attitudes can significantly affect the development, implementation, and perception of gene editing technologies. In some countries, where regulations may be more lenient, gene editing experiments may proceed without the same ethical oversight as in more regulated regions. This variance poses a challenge in creating a cohesive global approach to ensure responsible practices in gene editing.
Furthermore, international collaboration can foster a shared understanding of the ethical implications of CRISPR. By engaging in cross-border dialogues, scientists, ethicists, and policymakers can harmonize their approaches to gene editing, ensuring that scientific progress aligns with universal human rights and ethical values. Global initiatives aimed at establishing common guidelines for research and clinical use of CRISPR will be crucial to promote safety, transparency, and equity in healthcare worldwide.
Frequently Asked Questions
What are the ethical implications of CRISPR technology in gene editing regarding sickle cell disease?
The ethical implications of CRISPR technology in gene editing are significant, especially for diseases like sickle cell disease. While CRISPR has the potential to cure sickle cell by altering somatic cells, questions arise about the moral responsibility of changing human genetics. Key issues include health justice, as treatments may be cost-prohibitive and inaccessible to many, and the question of whether it’s ethical to edit genes for conditions compatible with life.
How does medical ethics relate to CRISPR gene editing and health justice?
Medical ethics plays a crucial role in the discussion of CRISPR gene editing. The advancement of CRISPR technology raises concerns about who gets access to such treatments, highlighting disparities in health justice. Ethical considerations must include the potential for benefitting only those who can afford advanced therapies, as well as the broader implications of editing genes that may redefine humanity’s understanding of normality and disability.
Are there risks associated with using CRISPR technology for genetic modification?
Yes, CRISPR technology carries several risks associated with genetic modification. These include potential unintended consequences from editing genes, as altering one gene can affect multiple biological processes due to the interdependent nature of genetics. There is also the concern of insufficient oversight, particularly in countries where regulations may be lax, leading to unethical experimentation.
Why is health equity a concern in the context of CRISPR gene editing?
Health equity is a significant concern in the context of CRISPR gene editing because the cost of treatments, such as those for sickle cell disease, can be exorbitant—exceeding $2 million. This high cost can create a divide where only wealthy individuals or nations can afford such advancements, exacerbating existing inequalities within global health systems and raising ethical questions about access to life-saving technologies.
What should be considered when making decisions about germline editing with CRISPR technology?
When considering germline editing with CRISPR technology, multiple factors should be assessed including the ethical implications of ‘designing’ children, parental rights in genetic choices, and potential societal impacts. Decisions must weigh the benefits of eliminating genetic diseases against the risks of creating new inequalities or altering human diversity, which could have profound implications for future generations.
How does CRISPR technology challenge concepts of ‘normal’ and identity within medical ethics?
CRISPR technology challenges traditional concepts of ‘normal’ and identity within medical ethics by allowing for the manipulation of genetic traits. This raises questions about what constitutes a disability or a ‘defect’ versus a natural variation in human genetics. The debate invites discussions on individual autonomy, societal values, and how we perceive variations in the human condition.
What are concerns regarding oversight in CRISPR gene editing practices globally?
Concerns regarding oversight in CRISPR gene editing practices globally include the potential for unethical research in countries with lenient regulations. Without strict oversight, there is a risk that scientists may attempt controversial or harmful genetic modifications without proper ethical considerations, leading to unintended consequences and societal backlash.
| Key Point | Details |
|---|---|
| Ethical Dilemmas of Gene Editing | The discussion revolves around whether we should modify human traits that define our humanity. |
| Crispr Technology | CRISPR can edit both somatic and germline genes, enabling potential cures for genetic diseases. |
| Practical Concerns | Cost of CRISPR treatments, such as $2.2 million for sickle cell, raises questions about accessibility and fairness. |
| Health Equity | There is concern about innovation exacerbating health disparities, benefiting the wealthy over the disadvantaged. |
| Parental Decision-Making | Should parents choose genetic modifications for traits like hearing ability? Raises questions of autonomy and ethics. |
| Global Oversight | Concerns about lack of regulation in countries conducting genetic research without oversight. |
| Unintended Consequences | Genetic modifications may lead to unforeseen health issues due to complex gene interactions. |
Summary
CRISPR ethical implications pose significant dilemmas that society must confront as gene-editing technology advances. The discourse surrounding whether we have the right or responsibility to alter human genetics raises profound moral questions. As scientists harness CRISPR for potential cures, the associated ethical considerations, such as accessibility, health equity, and the definition of human variation, cannot be overlooked. The medical community must navigate these concerns carefully, ensuring that innovation does not widen the chasm of inequality or lead to consequences that challenge the very essence of what it means to be human.